What is diabetes?
Diabetes is a medical condition characterized by elevated blood sugar (glucose) levels. It occurs when the pancreas produces insufficient insulin, fails to produce it entirely, or when the body does not respond effectively to insulin's actions. Affecting people across all age groups, diabetes is primarily a chronic condition, but it can be managed through medications, lifestyle modifications, or a combination of both.
Chronic types of diabetes include Type 1 diabetes, where the immune system attacks insulin-producing cells, and Type 2 diabetes, which develops when the body becomes resistant to insulin or fails to produce enough of it.
Additionally, there are potentially reversible forms of diabetes, such as prediabetes and gestational diabetes. Prediabetes is a state where blood sugar levels are higher than usual but not high enough to be classified as diabetes. Without intervention, prediabetes can progress to diabetes. Gestational diabetes occurs during pregnancy and typically resolves after childbirth, though it may increase the risk of developing Type 2 diabetes later in life.
Timely diagnosis and appropriate management are crucial to controlling diabetes and reducing the risk of complications.
What are the treatments for diabetes?
Comprehensive Management of Type 2 Diabetes
Managing Type 2 diabetes involves lifestyle changes, regular monitoring, and, if necessary, medication or insulin therapy. These measures aim to maintain blood sugar levels within a healthy range, minimizing the risk of complications and improving overall health.
Critical Aspects of Diabetes Management
1. Healthy Eating
While there isn’t a specific “diabetes diet,” certain dietary practices can help regulate blood sugar levels effectively:
- Structured meals: Maintain a regular schedule with balanced meals and healthy snacks.
- Smaller portions: Opt for controlled portion sizes.
- High-fibre foods: Include plenty of fruits, non-starchy vegetables, and whole grains.
- Reduced refined carbs: Limit refined grains, sugary foods, and starchy vegetables.
- Healthy fats: Use oils like olive or canola oil.
- Low-fat proteins: Choose lean meats, fish, and low-fat dairy products.
- Calorie management: Focus on consuming fewer calories for weight control.
Our registered dietitians can be invaluable in developing a personalized eating plan, identifying healthy food choices, and ensuring a well-balanced diet. They can also assist in monitoring carbohydrate intake to stabilize blood sugar levels.
2. Physical Activity
Regular exercise is essential for maintaining a healthy weight and managing blood sugar levels. Consult our healthcare providers before starting or modifying your workout routine.
- Aerobic Exercise: Walking, swimming, or cycling can improve cardiovascular health. Aim for 30 minutes daily or at least 150 minutes weekly.
- Resistance Training: Weightlifting, yoga, and other exercises enhance strength and balance. Aim for 2–3 sessions per week.
- Minimize Inactivity: Break up prolonged sitting with light activities every 30 minutes.
3. Weight Loss
Losing a small percentage of body weight (around 5%) can significantly improve blood sugar levels, cholesterol, and blood pressure. More considerable weight losses, up to 15%, provide even more significant benefits. Collaborate with our healthcare provider to set realistic weight-loss goals and develop sustainable lifestyle strategies.
4. Blood Sugar Monitoring
Regular blood sugar checks are crucial to ensure levels stay within target ranges. Monitoring can include:
- Blood glucose meters: Use a drop of blood to measure sugar levels.
- Continuous glucose monitoring (CGM): A sensor placed under the skin provides real-time data and alerts for fluctuations.
The testing frequency depends on your treatment plan and whether you use insulin.
5. Medications and Insulin Therapy
When lifestyle changes aren’t enough, your healthcare provider may prescribe medications or insulin to manage blood sugar levels:
- Oral medications like Metformin improve insulin sensitivity. Other options include sulfonylureas, glinides, and DPP-4 inhibitors.
- Injectable medications such as GLP-1 receptor agonists and insulin may be necessary for some patients.
Your provider will determine the best course of treatment, balancing efficacy with potential side effects.
Advanced Management Options
1. Weight-Loss Surgery
For individuals with a BMI of 35 or higher, weight-loss surgery may be an option to manage Type 2 diabetes. These procedures reduce food intake or nutrient absorption and often significantly improve blood sugar control. Surgery requires a lifelong commitment to dietary and lifestyle changes.
2. Pregnancy Considerations
People with Type 2 diabetes may need to adjust their treatment plans during pregnancy, including possible insulin therapy and regular eye checks for diabetic retinopathy.
Commitment to Lifelong Management
Effective management of Type 2 diabetes is a dynamic process requiring dedication to healthy habits, regular medical follow-ups, and a tailored treatment plan. By focusing on these elements, individuals can lead more nutritious lives and reduce the risk of complications.
Speak to our experts about diabetes.
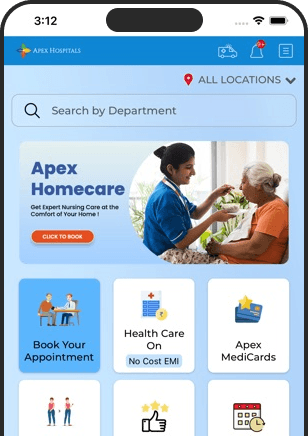
Managing diabetes requires personalized care and expert guidance to ensure optimal health outcomes. At Apex Hospitals, our team of diabetes specialists is here to provide you with comprehensive support, from tailored diet plans and exercise regimens to advanced treatment options like medication and insulin therapy. Our experts focus on understanding your unique needs, offering practical advice to help you maintain stable blood sugar levels and prevent complications. Whether you're newly diagnosed or looking to refine your management plan, we are dedicated to empowering you with the knowledge and tools needed for a healthier, more fulfilling life. Speak to our experts today to take control of your diabetes journey.
FAQS
Health In A Snap, Just One App.
KNOW MORE