Deep Brain Stimulation
Deep Brain Stimulation | Neurology | Apex Hospitals, Jaipur

What is deep brain stimulation (DBS)?
Deep brain stimulation (DBS) is a surgical procedure that involves implanting a device, similar to a pacemaker, into the brain to deliver electrical impulses to specific areas. These electrical impulses modulate the activity of targeted brain regions and can help alleviate symptoms of certain neurological conditions, particularly movement disorders.
DBS is primarily used to treat conditions including:
- Parkinson's disease
- Essential tremor
- Dystonia-related disorders like Miege syndrome
- Epilepsy
- Tourette syndrome
- Obsessive-compulsive disorder
Moreover, ongoing research is exploring the potential of deep brain stimulation as a therapeutic option for:
- Chorea, such as in Huntington's disease
- Chronic pain
- Cluster headache
- Dementia
- Depression
- Addiction
- Obesity
DBS is typically considered for individuals with movement disorders who have not responded adequately to medication or who experience significant medication-related side effects. While DBS does not cure these conditions, it can significantly improve the quality of life and reduce disability for many patients.
It's important to note that DBS is a complex procedure that carries risks, including surgical complications, infection, and side effects related to the stimulation. Candidates for DBS undergo a thorough evaluation by a multidisciplinary team of specialists to determine suitability for the procedure and to ensure that potential benefits outweigh the risks.
What are the risks of the procedure?
Possible side effects of deep brain stimulation (DBS) may include:
1. Seizures: DBS therapy can sometimes trigger seizures, although this is relatively rare.
2. Infection: There is a risk of infection at the site of the surgical incisions or around the implanted device.
3. Headache: Some individuals may experience headaches, particularly in the initial stages following surgery or during adjustments to the stimulation settings.
4. Confusion and trouble concentrating: DBS may cause cognitive side effects in some individuals, such as confusion, difficulty concentrating, or memory problems.
5. Stroke: While uncommon, DBS surgery carries a risk of stroke, mainly if there is bleeding in the brain during the procedure.
6. Hardware complications: Complications related to the implanted hardware, such as lead migration, device malfunction, or erosion of the lead wire, may occur.
7. Temporary pain and swelling at the implantation site: It is expected to experience temporary discomfort or swelling at the site where the electrodes are implanted.
8. Numbness or tingling sensations: Some individuals may experience numbness or tingling in the areas surrounding the implanted electrodes.
9. Muscle tightness or weakness: DBS therapy may lead to muscle tightness or weakness, particularly in the face or limbs.
10. Speech difficulties: In some cases, DBS can affect speech, causing changes in voice quality, articulation difficulties, or other speech-related issues.
11. Balance problems: DBS may impact balance and coordination in some individuals, leading to difficulties with walking or maintaining posture.
12. Light-headedness: Some people may experience feelings of light-headedness or dizziness, particularly during or after adjustments to the stimulation settings.
13. Vision changes: DBS can sometimes cause changes in vision, including double vision or other visual disturbances.
14. Mood changes: Mood changes, including feelings of anger, mania, or depression, may occur as a result of DBS therapy.
It's important to note that not everyone will experience these side effects, and their severity can vary from person to person. Additionally, many side effects are temporary and can often be managed with adjustments to the stimulation settings or other interventions. Individuals considering DBS should discuss the potential risks and benefits with their healthcare provider.
How can you prepare for Deep brain stimulation (DBS)?
First, consider the pros and cons. Deep brain stimulation is a significant and potentially hazardous procedure. If you qualify for it, evaluate the risks and potential benefits in consultation with your healthcare team.
Next, get ready for surgery. Before the procedure, you'll probably undergo medical tests to ensure that deep brain stimulation is a suitable and safe choice. Brain-imaging studies, like an MRI, may also be necessary before surgery to map out the areas of your brain where the electrodes will be implanted.
Procedure Details
During the procedure:
Here's a breakdown of how deep brain stimulation surgery generally works:
1. Brain Surgery:
Your care team begins by fitting you with a unique head frame called a stereotactic head frame to keep your head still during the procedure. Neuroimaging, such as a brain MRI or CT scan, is then used to map your brain and identify the precise area for electrode placement.
a. Electrode Placement: Most often, electrodes are implanted while you're awake to ensure the effects of stimulation can be thoroughly tested. Local anaesthesia is typically administered to numb your scalp. The surgeon carefully implants thin wire leads with electrodes at the tips into specific areas of your brain. In some cases, leads are placed on both sides of the brain. A wire is then routed under your skin to a pulse generator implanted near your collarbone.
b. Monitoring: During surgery, the neurologist and surgeon monitor your brain to ensure accurate electrode placement.
2. Chest Wall Surgery:
In the second part of the surgery, the surgeon implants the pulse generator under the skin of your chest, usually near the collarbone. This device contains the batteries needed for stimulation. General anaesthesia is used during this procedure. Wires from the brain electrodes are routed under your skin and connected to the pulse generator.
a. Programming: Several weeks after surgery, the pulse generator is activated during an appointment with your healthcare professional. It can also be programmed externally using a special remote control. The stimulation settings are customized to your condition, and they may take several months to optimize.
After the procedure
After surgery, you have control over the generator and can turn it on or off using the remote control. The stimulation may be continuous or adjusted based on your condition. The battery life varies and will need replacement when depleted, typically done during an outpatient procedure.
Speak to our experts about deep brain stimulation
Speak to our experts about deep brain stimulation and discover how this innovative procedure can transform your life. Whether you're considering it for Parkinson's disease, essential tremor, or other neurological conditions, our team of specialists is here to provide personalized guidance and answer all your questions. Take the first step towards a brighter future by scheduling a consultation with us today. Your journey to improved quality of life starts here.
FAQS
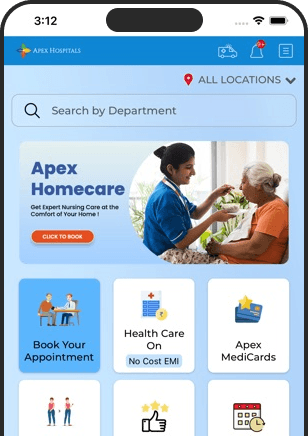
Health In A Snap, Just One App.
KNOW MORE