Epilepsy
What is epilepsy?
Epilepsy is a chronic disease characterized by recurrent seizures, which are sudden and uncontrolled electrical disturbances in the brain. These seizures can manifest in various ways, ranging from brief lapses of attention to severe convulsions. Epilepsy is not a single disease but a broad term encompassing numerous conditions that share the common feature of seizures.
Epilepsy affects people of all ages, races, and socioeconomic backgrounds, and its impact can be far-reaching, influencing not only the individual but also their family, friends, and community. Although epilepsy is a chronic condition, with proper diagnosis and treatment, many individuals can achieve seizure control and lead fulfilling lives.
Common causes of epilepsy
Epilepsy can arise from a wide range of underlying causes, some of which are:
1. Genetic factors: Certain genetic mutations or inherited conditions can predispose an individual to epilepsy.
2. Brain injuries: Head trauma, stroke, brain tumours, or infections affecting the brain can disrupt regular neuronal activity and lead to seizures.
3. Developmental disorders: Conditions such as autism, Down syndrome, and other developmental disabilities can increase the risk of epilepsy.
4. Metabolic disorders: Imbalances in electrolytes, hormones, or other metabolic processes can trigger seizures in some individuals.
5. Brain infections: Infections can include brain abscess, meningitis, encephalitis, and neurocysticercosis.
Understanding the different types of epilepsy
Epilepsy is a heterogeneous condition, with various types classified based on the location of seizure onset, the underlying cause, and the pattern of seizures. Some of the most common types include:
1. Generalized epilepsy: Seizures originate from both hemispheres of the brain simultaneously. Examples include tonic-clonic seizures (grand mal seizures) and absence seizures (petit mal seizures).
2. Focal epilepsy (partial seizures): Seizures begin in a specific area or network of the brain. These can be further classified as simple partial seizures (without loss of consciousness) or complex partial seizures (with impaired consciousness).
3. Childhood epilepsy syndromes: Certain types of epilepsy are specific to childhood and have distinct clinical features, such as Lennox-Gastaut syndrome, Dravet syndrome, and infantile spasms.
Symptoms of epilepsy
The symptoms of epilepsy can vary widely depending on the type of seizure and the area of the brain affected. Some common symptoms include:
- Episodes of temporary awareness or consciousness loss.
- Involuntary muscle movements, jerking, or loss of muscle tone.
- A vacant stare or "staring into space" appearance.
- Brief confusion, slowed thinking, and difficulties in speaking and understanding.
- Changes in hearing, vision, taste, smell, and sensations of numbness or tingling.
- Challenges with speaking or understanding.
- Gastrointestinal discomfort, sensations of heat or cold, and goosebumps.
- Repetitive behaviours like lip-smacking, chewing, hand rubbing, or finger movements.
- Psychological symptoms such as fear, dread, anxiety, or déjà vu.
- Increased heart rate and breathing rate.
What are seizure triggers?
Seizure triggers are factors or events that precede the onset of a seizure.
Commonly reported seizure triggers include:
- Stress.
- Sleep issues include poor sleep quality, insufficient sleep, fatigue, disrupted sleep, and sleep disorders like sleep apnea.
- Alcohol consumption, alcohol withdrawal, or recreational drug use.
- Hormonal changes, including menstrual hormonal fluctuations.
- Illness or fever.
- Exposure to flashing lights or patterns.
- Poor dietary habits include imbalanced meals or inadequate fluid intake, vitamin and mineral deficiencies, and meal skipping.
- Physical exhaustion.
- Specific foods (caffeine is often cited as a trigger).
- Dehydration.
- Certain times of the day or night.
- Use of particular medications; for instance, diphenhydramine found in some over-the-counter colds, allergies, and sleep aids is reported as a trigger.
- Missed doses of anti-seizure medications.
Diagnostic tests for epilepsy
To diagnose epilepsy and determine its underlying cause, healthcare professionals may employ various diagnostic tests, including:
1. Electroencephalogram (EEG): This test measures and records the brain's electrical activity, helping to identify abnormal patterns associated with seizures.
2. Neuroimaging techniques: Magnetic resonance imaging (MRI) and computed tomography (CT) scans can reveal structural abnormalities or lesions in the brain that may be causing seizures.
3. Blood tests: Certain blood tests can help rule out metabolic or genetic disorders that may contribute to epilepsy.
4. Neuropsychological testing: These assessments evaluate cognitive, behavioural, and emotional functioning, which can be affected by epilepsy and its treatments.
Treatment for epilepsy
The primary goal of epilepsy treatment is to achieve seizure control while minimizing side effects and maintaining an optimal quality of life. Treatment options may include:
1. Medications for managing seizures
Anti-seizure medications, also known as antiepileptic drugs (AEDs), are the first-line treatment for most types of epilepsy. These medications work by altering the electrical activity in the brain and reducing the likelihood of seizures.
2. Surgical interventions for epilepsy
In some cases, when medications are ineffective or cause intolerable side effects, surgical interventions may be considered. These procedures aim to remove or isolate the area of the brain responsible for generating seizures. Standard surgical options include:
- Resective surgery: Removal of the brain tissue responsible for causing seizures.
- Disconnection surgery: Severing the connections between the seizure-generating area and the rest of the brain.
- Neuromodulation therapies: Implantation of devices that deliver electrical stimulation to specific brain regions to disrupt seizure activity.
Surgical interventions are typically reserved for individuals with drug-resistant epilepsy and require careful evaluation by a multidisciplinary team of specialists.
3. Lifestyle modifications to manage epilepsy
In addition to medical and surgical treatments, lifestyle modifications can play a crucial role in managing epilepsy and reducing the risk of seizures. These may include:
- Maintaining a regular sleep schedule
- Reducing stress and anxiety through relaxation techniques
- Adopting a balanced and nutritious diet
- Engaging in regular physical activity (as recommended by healthcare providers)
- Avoiding potential seizure triggers, such as flashing lights or sleep deprivation
FAQS
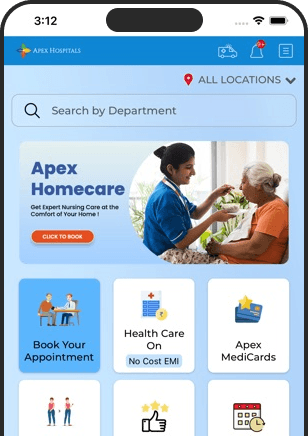
Health In A Snap, Just One App.
KNOW MORE