Percutaneous Discectomy/ Nucleoplasty
Percutaneous Discectomy/ Nucleoplasty Surgery

Percutaneous Discectomy (Nucleoplasty)
Percutaneous discectomy, or nucleoplasty, is a fluoroscopic image-guided, minimally invasive discectomy procedure. This procedure treats herniated disc-related leg, arm, chest, or buttock discomfort.
During percutaneous discectomy, a doctor removes a small quantity of disc tissue under image guidance. This reduces pain and restores mobility by releasing pressure from the nerves. Typically, the procedure takes one hour.
Who would benefit from percutaneous discectomy?
Candidates for percutaneous discectomy suffer from chronic pain caused by a herniated disc compressing a spinal nerve. This treatment is most effective for patients with radiating discomfort in the arms, legs, chest, or buttocks.
This procedure is generally less effective for patients who only experience back or neck discomfort.
A physician may suggest percutaneous discectomy if:
- After 6 to 12 weeks, conservative treatments such as physical therapy and steroid injections have failed to ease the symptoms.
- A patient has difficulty standing or walking due to nerve dysfunction.
- Pain radiates into the legs, arms, chest, or buttocks and has become too intense to bear.
How is the percutaneous discectomy procedure done?
Most of the time, percutaneous discectomy is administered as a minimally invasive procedure.
During the procedure, the doctor makes a microscopic puncture in the annulus, the outer lining of the herniated disc. The doctor then uses tiny instruments to remove a portion of the extra soft gelatinous material from within the disc. This material is the nucleus pulposus of the disc.
This procedure reduces the size of the protruding disc, thereby alleviating the excruciating pressure on the affected spinal nerve. In an ambulatory surgery setting, the process typically lasts an hour.
What are the potential risks and complications associated with percutaneous discectomy?
Even minimally invasive interventions carry some degree of danger. Potential complications include but are not limited to the following:
- Infection
- Bleeding
- Nerve damage
- Blood vessel damage
- Worsening discomfort
This procedure can be performed in various methods, each with potential risks and complications. Patients should discuss these hazards with their doctor about the specific procedure they are contemplating.
What advantages does percutaneous discectomy offer?
Patients experience pain relief, a decreased need for pain medication, and an increased capacity to engage in normal daily activities.
Studies have shown minimal complication rates for this outpatient procedure versus spine surgery alternatives.
How long does percutaneous discectomy recovery take?
As each individual is unique, recovery durations may vary. However, most patients return home within a few hours of their outpatient procedure.
When can I return to school or work following percutaneous discectomy?
The timing of a return to work is contingent on the procedure performed and the patient's occupation and lifestyle. A physician will consider a patient's anticipated lifting, strolling, and sitting activities.
Depending on their doctor's instructions, patients can typically return to work within three to five days following the procedure.
After a percutaneous discectomy procedure, what precautions should I take?
The decompression of discs percutaneously can provide pain relief. However, this relief might be temporary. This is because the procedure does not treat the root cause of the herniated disc.
Achieving and maintaining a healthy weight is essential to reduce disc tension. To prevent re-injury, patients should limit themselves to low-impact exercises. Additionally, they should restrict repetitive bending, twisting, or hauling.
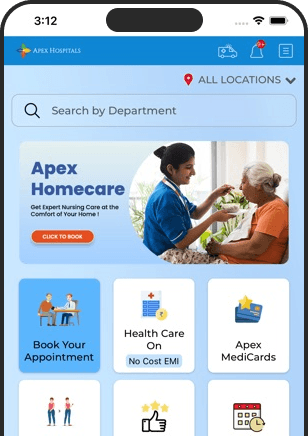
Health In A Snap, Just One App.
KNOW MORE