What exactly is mechanical ventilation?
Mechanical ventilation is a type of life support that allows you to breathe (ventilate) when you cannot do so on your own. This can happen during surgery or when you're extremely ill. While mechanical ventilation cannot treat illnesses directly, it can keep you stable while other therapies and medications help your body heal.
What exactly is a ventilator?
A ventilator is a machine that assists you in breathing. The ventilator, like crutches, either partially or entirely supports your lung functions. A ventilation system:
- It delivers oxygen to your lungs.
- Aids in the removal of carbon dioxide (CO2) from the lungs.
- Provides pressure to keep the little air sacks (alveoli) in your lungs from collapsing.
- Providers can modify the machine's settings to match your requirements.
What are the different methods of mechanical ventilation?
Modern mechanical ventilators use positive pressure to pump air into your lungs. Positive pressure ventilation can be either invasive or non-invasive.
Invasive mechanical ventilation means you have a tube in your airway connected to a ventilator. This tube can be inserted into your mouth (intubation) or neck (tracheostomy).
Non-invasive ventilation: It involves the use of a face mask attached to a ventilator. Straps secure the mask to your face. The ventilator pushes air into your lungs.
What is the purpose of mechanical ventilators?
Providers employ mechanical ventilators to assist you when you cannot breathe independently. Ventilation using mechanical means:
- Can provide you with oxygen.
- Aids in the removal of carbon dioxide so that it does not accumulate.
- Stops sections of your lungs from collapsing due to a lack of pressure.
Who requires mechanical ventilation?
You may require mechanical respiration:
- During the surgery: General anaesthesia might make it difficult to breathe normally.
- If you have certain lung diseases or infections.
- In case of a medical emergency, when something clogs your airway or makes breathing difficult.
- Suppose you have specific brain injuries or conditions. Your brain may not connect well with the rest of your body, especially your lungs, preventing you from breathing normally.
- If you have a condition that causes your blood to contain too much carbon dioxide (hypercapnia) or insufficient oxygen (hypoxemia), you should consult your doctor.
- Aspiration: To keep fluids from unintentionally entering your lungs.
How long may you be kept on a mechanical ventilator?
The reason determines the duration of mechanical ventilation. It could be hours, days, weeks, months, or even years. You should only be on a ventilator for as little time as possible. Your providers will assess your ability to breathe on your own daily or more frequently.
If you need to be on a ventilator for an extended period (two weeks or more), a provider will move you from an endotracheal tube to a tube in your neck (tracheostomy).
How is invasive mechanical ventilation imposed?
A provider will initiate invasive mechanical ventilation by:
- You will be given drugs to relax (sedation) and keep you from moving (paralysis). You'll most likely be sedated throughout the procedure, but the paralytic will wear off once you're on the ventilator.
- Insert an endotracheal (ET) tube into your throat and trachea (the airway that leads to your lungs).
- Connect the tubing to the ventilator. The ventilator will assist you in breathing until your medical team determines it is safe to do it again.
These are the general procedures for kicking off mechanical ventilation. Some of these measures may alter depending on your scenario, mainly whether it is an emergency.
What happens when you're on a breathing machine?
Providers will undertake additional treatments to treat or avoid complications while you are on a ventilator. These are some examples:
- Monitoring.
- Suctioning.
- Providing medicines
- We are providing fluids and nutrients.
- Mobilization.
- Bronchoscopy.
When you're on a ventilator, who looks after you?
You are treated in the critical care unit (ICU) when you require mechanical ventilation. They may keep a tight eye on you there. All ICU providers are highly educated to care for patients who require mechanical ventilation. Providers who may be able to help you include:
- Respiratory Therapists.
- Anaesthesiologists, pulmonologists, and critical care physicians.
- Nurse practitioners
- Registered nurses
- Nurse aides
### What are some of the benefits of mechanical ventilation?
Mechanical ventilation has the following advantages:
- Breathing does not need any effort. Your body can concentrate on healing from infections or other ailments.
- It supplies all of the oxygen you require while also removing carbon dioxide.
- It generates pressure to keep your lungs' tiny sacs from collapsing.
- It keeps your lungs open.
What are the risks associated with mechanical ventilation?
Providers avoid mechanical ventilation difficulties. However, there may be some hazards, such as:
- Infections caused by bacteria: Bacteria can enter your lungs through the tube in your airways, causing illnesses such as ventilator-associated pneumonia (VAP). Antibiotics are used to treat this.
- Damage to the lungs: The ventilator's pressure can harm your lungs
- Collapsed lungs: If a section of your lung is weak, it may develop a hole and collapse (pneumothorax).
- Changes in the heart and blood flow: Being on a ventilator might impact how your heart works. If your heart isn't working correctly, it can lower your blood pressure or increase your heart rate. These alterations may also result in less oxygen reaching your blood (decreased perfusion) despite plenty of getting to your lungs.
- People are sometimes unable to take off a ventilator. If you need to be on a ventilator for an extended period, your tube will be removed from your mouth. A tube will be inserted through a small cut (incision) in your neck.
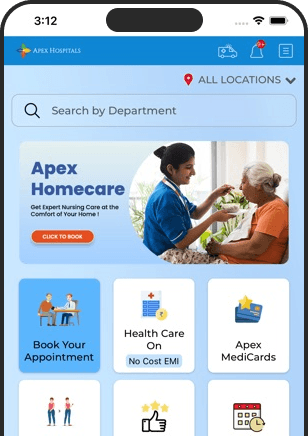
Health In A Snap, Just One App.
KNOW MORE