Intubation

What is intubation?
Intubation is when a healthcare worker puts a tube into a person's mouth or nose and subsequently into their trachea (airway/windpipe). The tube keeps the trachea open, allowing air to pass through. The tube can be connected to an air or oxygen delivery unit.
Intubation is also known as tracheal or endotracheal intubation.
Why would someone require intubation?
Intubation is required when your airway is clogged or damaged, or you cannot breathe independently. The following are some common conditions that might lead to intubation:
- Airway obstruction (anything trapped in the airway that prevents airflow).
- Cardiac arrest is an abrupt loss of heart function.
- A neck, abdomen, or chest injury or trauma that affects your airway.
- A loss of awareness or a low level of consciousness causes a person to lose control of their airway.
- Requirement of surgery that can make you unable to breathe on your own.
- Apnoea (a momentary cessation of breathing) or respiratory failure.
- The risk of aspiration (breathing in an object or substance such as food, vomit, or blood).
What is the distinction between being intubated and being ventilated?
Being intubated and being on a ventilator are connected but not identical.
The process of placing an endotracheal tube (ETT) into the airway (windpipe) is called intubation. The tube is subsequently connected to an air-delivery apparatus. A ventilator is a machine that blows oxygen into your airway and lungs. It might be a bag that a healthcare worker squeezes to push air into your body. A ventilator may sometimes distribute air through a mask rather than a tube.
Who should not have an intubation?
In rare situations, healthcare personnel may conclude that intubation is unsafe, such as when there is severe trauma to the airway or an obstruction that prevents safe tube installation.
In such circumstances, your doctor may surgically open your airway via your throat at the base of your neck. This is referred to as tracheostomy. A tracheostomy is often required when you have an endotracheal tube in place for more than a few days or are expected to have it for weeks.
What is the procedure for endotracheal intubation?
The majority of intubation procedures take place in a hospital. Emergency medical services (EMS) staff may intubate patients outside the hospital.
Healthcare providers will do the following during the procedure:
- Put an IV needle in your arm.
- Anaesthesia is the administration of drugs through an IV to put you to sleep and avoid pain throughout the surgery.
- Put an oxygen mask over your nose and mouth to provide extra oxygen.
- Remove the mask.
- Tilt your head back and insert a laryngoscope into your mouth (or, if required, your nose). The instrument features a handle, LEDs, and a dull blade to assist the healthcare provider in guiding the tracheal tube.
- Avoiding your teeth, move the instrument toward the rear of your mouth.
- Raise the epiglottis, a tissue flap hanging in the mouth's rear to protect the larynx (voice box).
- Insert the laryngoscope tip into your larynx and then into your trachea.
- Inflate a tiny balloon around the endotracheal tube to ensure that it remains in the trachea and that all air administered through the tube reaches the lungs.
- Take out the laryngoscope.
- Use tape around your mouth or a strap around your head to keep the tracheal tube in place.
- Check that the tube is in the correct position. This can be accomplished by obtaining an X-ray or forcing air into the tube through a bag and listening for breath sounds.
Is it possible to chat or eat while intubated?
Because the endotracheal tube travels through your vocal cords, you cannot talk.
You also can't eat or drink when intubated because you can't swallow. Depending on how long you'll be intubated, your healthcare providers may provide you with nutrition via IV or IV fluids or a separate slender tube inserted through your mouth or nose, ending in your stomach or small bowel.
During extubation, how is the tracheal tube removed?
When the healthcare providers determine that removing the tube is safe, they will do it. This is a simple procedure known as extubation. They are going to:
- Take off the tape or strap that is holding the tube in place.
- Remove any debris from the airway with a suction device.
- Remove the balloon from your trachea.
- Ask you to take a big breath, then cough or exhale while they remove the tube.
- Your throat may be uncomfortable for a few days following extubation, and you may have difficulty speaking.
What are the risks of intubation?
Intubation is a routine and generally safe treatment that can aid in saving a person's life. The majority of people recover in a few hours or days; however, some unusual problems can occur:
- Aspiration: When intubated, they may inhale vomit, blood, or other fluids.
- Endobronchial intubation: The tracheal tube may be sent down one of two bronchi connecting your trachea to your lung. This is also referred to as mainstem intubation.
- If the tube reaches your oesophagus (food tube) instead of your trachea, it can cause brain damage or even death if not discovered quickly.
- Failure to secure the airway: If intubation fails, healthcare providers may be unable to treat the patient.
- Infections: Intubated patients may develop infections such as sinus infections.
- Injury: The procedure has the potential to cause damage to your mouth, teeth, tongue, voice chords, or airway. The injury could result in bleeding or swelling.
- Problems after anaesthesia: While most people recover successfully, some have difficulty waking up or experience medical issues.
- Tension pneumothorax: When air becomes trapped in your chest cavity, your lungs can collapse.
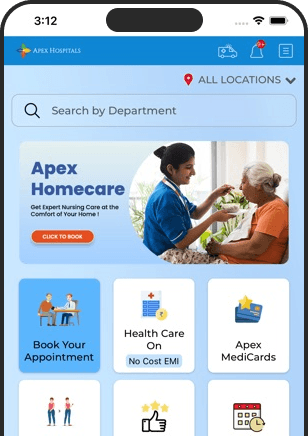
Health In A Snap, Just One App.
KNOW MORE