Understanding Parkinson's Disease: Causes, Symptoms, and Management Strategies
By:

Apex Hospitals
12-07-2023 5 Min Read
Parkinson's disease is a degenerative brain disorder affecting millions worldwide. It is a chronic condition that gradually worsens over time, leading to physical and cognitive symptoms. Understanding Parkinson's disease is crucial for patients and caregivers, as it can significantly impact the quality of life.
What is Parkinson’s disease?
Parkinson's disease is a neurodegenerative disorder that primarily affects the dopamine-producing neurons in the brain. Dopamine is a neurotransmitter that is crucial in regulating movement and coordination. Dopamine is produced in a brain region termed the "substantia nigra." In Parkinson's disease, substantia nigra cells begin to die. When this occurs, dopamine levels decline. When they have decreased by 60 to 80 per cent, Parkinson's symptoms appear.
Causes of Parkinson’s disease
The exact parkinsons disease causes is still unknown, but researchers believe that a combination of genetic and environmental factors may contribute to its development. Some scientists believe viruses can also cause Parkinson's disease.
Parkinson's has been linked to low levels of dopamine and norepinephrine, a substance that regulates dopamine. Lewy bodies which are abnormal proteins, have also been discovered in the brains of Parkinson's patients. Scientists do not know if Lewy bodies contribute to the development of Parkinson's disease.
While there is no known cause, research has identified the following categories of individuals who are more likely to develop the condition:
- Sex: Men are 1.5 times more likely than women to develop Parkinson's disease.
- Race: Parkinson's disease is more prevalent among whites than among African-Americans or Asians, according to research. Geography may be one cause of an increased risk.
- Age: Parkinson's disease typically manifests between 50 and 60. Approximately four per cent of cases occur before the age of 40.
- Family background: People with close relatives who have Parkinson's disease are more likely to develop the disease themselves.
- Toxins: Certain toxins may increase the likelihood of developing Parkinson's disease.
- Head trauma: People who sustain head injuries may have an increased risk of developing Parkinson's disease.
However, more research is needed to fully understand the complex interplay between genetics and the environment in Parkinson's disease.
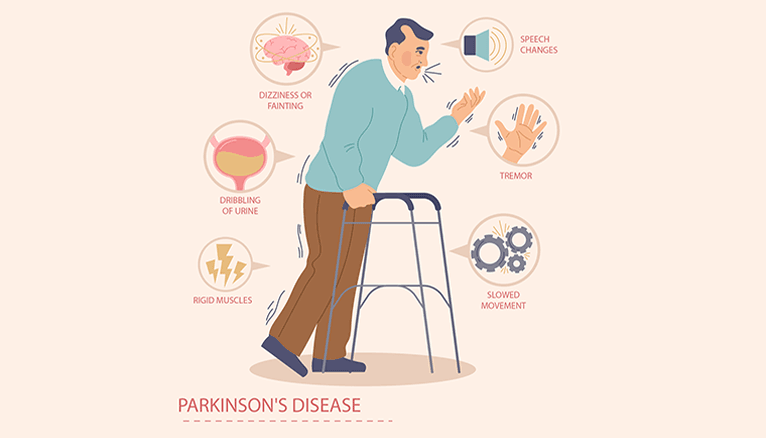
Symptoms of Parkinson's Disease
The parkinsons disease symptoms can vary from person to person, but the most common ones include:
- Tremors: Tremors are uncontrollable movements that typically start in the hands or fingers. They often occur when the affected person rests and tend to disappear during movement.
- Bradykinesia: Bradykinesia refers to slowness of movement. People with Parkinson's disease may have difficulty initiating movements, making simple tasks like getting out of bed or buttoning a shirt challenging.
- Stiffness: Stiffness, also known as rigidity, is another hallmark symptom of Parkinson's disease. It can make muscles feel tight and limit the person's range of motion.
- Postural instability: Parkinson's disease can also affect a person's balance and coordination, making it difficult to maintain an upright posture and increasing the risk of falls.
In addition to these primary symptoms, Parkinson's disease can cause various secondary symptoms, including depression, anxiety, sleep disturbances, and cognitive changes.
Diagnosis and Stages of Parkinson's Disease
Diagnosing Parkinson's disease can be challenging, as no specific test can confirm its presence. Instead, doctors rely on a combination of medical history, physical examination, and the presence of characteristic symptoms. They may also order additional tests, such as brain imaging scans such as CT Scan or MRI, to rule out other conditions that may cause similar symptoms.
Stages:
Once diagnosed, Parkinson's disease is typically classified into five stages based on the severity of symptoms and their impact on daily life.
Stage 1:
Stage 1 Parkinson’s is mildest. It's so mild you may not detect symptoms. They may not yet disrupt your routine.
Symptoms may be limited to one side of the body.
Stage 2:
The transition between stages 1 and 2 can take months or even years. Each person will have a unique experience. At this stage, you may experience the following symptoms:
- Muscle rigidity
- tremors
- facial expression changes
- trembling
There may be symptoms on both sides of the body.
Stage 3:
Mid-stage symptoms change. Symptoms may be more evident but unlikely to change. They can also disrupt your routine. Slower movements slow activities. Falls increase when balance issues worsen. Stage 3 Parkinson's patients may usually execute tasks independently.
Stage 4:
Stage 3 through 4 varies significantly. Without a walker, you'll have trouble standing. Muscles and reactions slow down too. Living alone can be unsafe.
Stage 5:
In this final stage, the symptoms are severe and require constant care. Standing may be impossible. Wheelchairs are always needed. Parkinson's patients may also have disorientation, delusions, and hallucinations.
Management Strategies for Parkinson's Disease
While there is no cure for Parkinson's disease, various management strategies can help control symptoms and improve quality of life. These strategies typically involve a combination of medications, surgical parkinson's disease treatments, lifestyle changes, and therapies.
- Medications for Parkinson's Disease
- Medications are often prescribed to increase dopamine levels in the brain or mimic its effects. Levodopa, dopamine agonists, and MAO-B inhibitors commonly manage motor symptoms. However, it is essential to note that medications may have side effects, and their effectiveness may diminish over time.
- Surgical Treatments for Parkinson's Disease
- Surgical treatments, such as deep brain stimulation, may be recommended for individuals who do not respond well to medication or experience severe motor fluctuations. Deep brain stimulation involves implanting electrodes in specific brain areas to regulate abnormal electrical signals and alleviate symptoms.
- Lifestyle Changes and Therapies for Parkinson's Disease
- In addition to medications and surgery, specific lifestyle changes and therapies can also help manage Parkinson's disease. Regular exercise, such as walking or swimming, can improve muscle strength and flexibility, while physical and occupational therapy can help individuals maintain independence in daily activities. Speech therapy and support groups can also be beneficial in managing communication difficulties and providing emotional support.
While there is no cure, advancements in research and treatment options offer hope for better symptom management and improved quality of life. By staying informed, seeking appropriate medical care, and implementing lifestyle changes, individuals with Parkinson's disease can optimize their well-being and lead fulfilling lives.
Related Articles
Connect With Us
Health In A Snap, Just One App.
KNOW MORE